The Emerging Practice of Integrated Care in Senior Communities
Introduction
Addressing the medical needs of residents adds value to senior communities. This article is written to encourage senior communities to provide the “integrated model” of care, which represents onsite medical care. Such diversity is healthy, and consistent with the way the assisted living industry has evolved in meeting the needs of an aging U.S. population.
The Challenge
Many senior community residents are frail and medically complex. Most need help with activities of daily living (ADLs), and often have some degree of dementia. Although the health care needs of residents have progressed over the last several decades, the senior housing industry in many parts of the country has been slow to address those needs.
Senior communities embrace the “social” or “hospitality” model of service, which emphasizes life-style considerations and hotel-type services. AL communities also provide 24-hour staffing, assistance with ADLs, and social activities. More recently, senior communities have emphasized the need to become more person-centered, by providing on-demand dining services, and enhanced technology. Some make ancillary services, such as physical therapy, available onsite to their residents also.
But the “hospitality” or “social” service model does not address the medical care needs of residents, or their mental health issues. Aging-in-place is of great importance to older individuals, especially the “silver tsunami” of aging baby boomers. Older adults prefer living in a home-like environment, up until and including the end-of-life. Few people want to spend their last weeks or months of life in a hospital or nursing home.
Studies have confirmed that senior communities that meet the medical needs of their residents experience less resident turnover, and higher facility occupancy. This is not surprising, since the most common reason for resident attrition is health-related, mainly the transfer to “higher” levels of care.
Health-related turnover in AL communities is an astonishing 55% annually, not including death.
The Path Forward
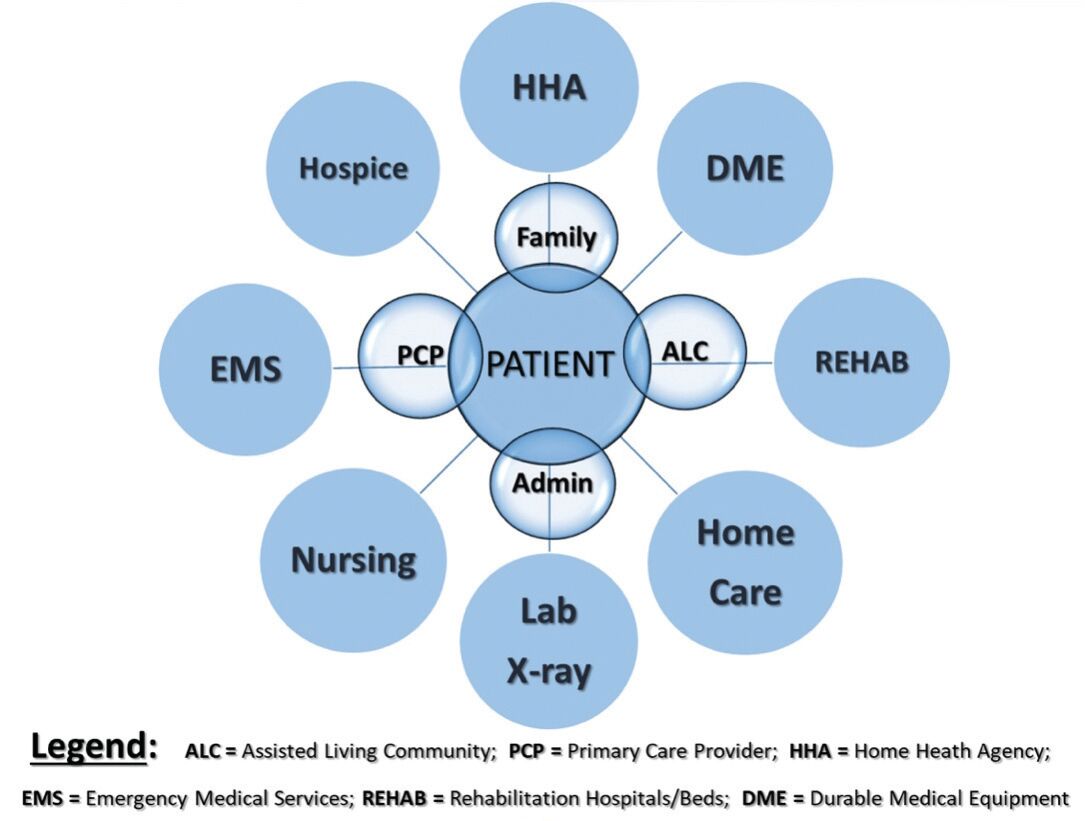
The “integrated model” of care refers to primary care services provided on-site in the community, by clinicians skilled in caring for complex older patients complemented by the services of home health agencies, durable medical equipment providers, hospice and palliative care clinicians, as well as medical imaging or laboratory testing.
For example, my practice – Doctors Making Housecalls (DMHC) – employs 90+ clinicians (50 doctors and 40 advanced practitioners), who are supported by 140 administrative personnel from our headquarters office. We serve residents in more than 250 senior communities across North Carolina, visiting each community once or twice a week. Consistent with our commitment to provide “proactive” care, our clinicians see patients often (an average of once every 5 weeks) and spend far more time on each visit than clinicians can afford to spend in the typical “brick and mortar” practice. Our clinician visits are based entirely on the medical needs of our patients.
Except for deductibles and co-pays, which apply to physician visits in every location, Medicare pays for all the above services. In addition to DMHC, there are practices and clinicians providing similar services throughout NC.
The integrated model reduces the need for travel to a doctor’s office or urgent care clinic, trips that are often associated with long waits for care, and short visits with the doctor.The Centers for Medicare & Medicaid Services (CMS) have reported that onsite care reduces emergency room visits, hospitalizations, and hospital readmissions – by an average of 55% that saves money, both for “the system,” and for the patient.
Onsite care not only saves money, it also reduces disruptions in the resident’s normal routine and that of their loved ones and caregivers.